House Call
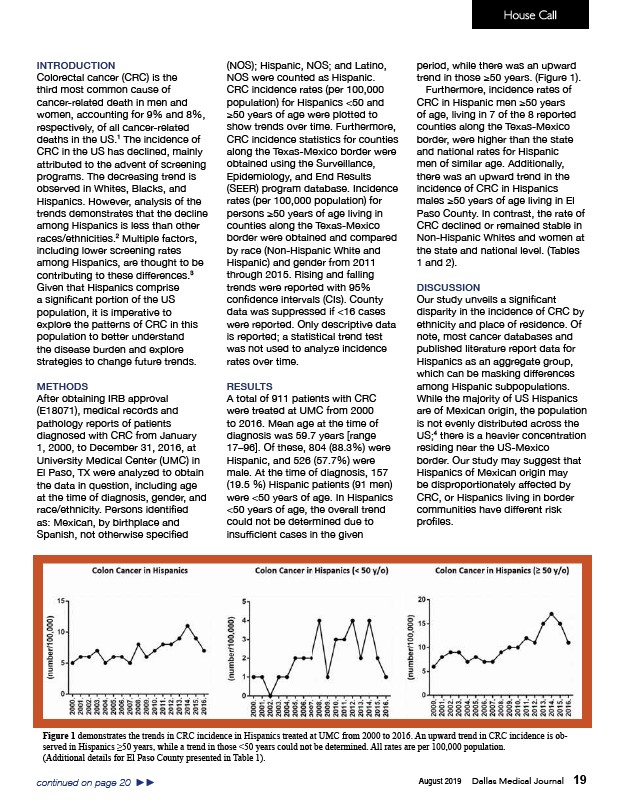
Figure 1 demonstrates the trends in CRC incidence in Hispanics treated at UMC from 2000 to 2016. An upward trend in CRC incidence is observed
in Hispanics ≥50 years, while a trend in those <50 years could not be determined. All rates are per 100,000 population.
August 2019 Dallas Medical Journal 19
INTRODUCTION
Colorectal cancer (CRC) is the
third most common cause of
cancer-related death in men and
women, accounting for 9% and 8%,
respectively, of all cancer-related
deaths in the US.1 The incidence of
CRC in the US has declined, mainly
attributed to the advent of screening
programs. The decreasing trend is
observed in Whites, Blacks, and
Hispanics. However, analysis of the
trends demonstrates that the decline
among Hispanics is less than other
races/ethnicities.2 Multiple factors,
including lower screening rates
among Hispanics, are thought to be
contributing to these differences.3
Given that Hispanics comprise
a significant portion of the US
population, it is imperative to
explore the patterns of CRC in this
population to better understand
the disease burden and explore
strategies to change future trends.
METHODS
After obtaining IRB approval
(E18071), medical records and
pathology reports of patients
diagnosed with CRC from January
1, 2000, to December 31, 2016, at
University Medical Center (UMC) in
El Paso, TX were analyzed to obtain
the data in question, including age
at the time of diagnosis, gender, and
race/ethnicity. Persons identified
as: Mexican, by birthplace and
Spanish, not otherwise specified
(NOS); Hispanic, NOS; and Latino,
NOS were counted as Hispanic.
CRC incidence rates (per 100,000
population) for Hispanics <50 and
≥50 years of age were plotted to
show trends over time. Furthermore,
CRC incidence statistics for counties
along the Texas-Mexico border were
obtained using the Surveillance,
Epidemiology, and End Results
(SEER) program database. Incidence
rates (per 100,000 population) for
persons ≥50 years of age living in
counties along the Texas-Mexico
border were obtained and compared
by race (Non-Hispanic White and
Hispanic) and gender from 2011
through 2015. Rising and falling
trends were reported with 95%
confidence intervals (CIs). County
data was suppressed if <16 cases
were reported. Only descriptive data
is reported; a statistical trend test
was not used to analyze incidence
rates over time.
RESULTS
A total of 911 patients with CRC
were treated at UMC from 2000
to 2016. Mean age at the time of
diagnosis was 59.7 years range
17–96. Of these, 804 (88.3%) were
Hispanic, and 526 (57.7%) were
male. At the time of diagnosis, 157
(19.5 %) Hispanic patients (91 men)
were <50 years of age. In Hispanics
<50 years of age, the overall trend
could not be determined due to
insufficient cases in the given
period, while there was an upward
trend in those ≥50 years. (Figure 1).
Furthermore, incidence rates of
CRC in Hispanic men ≥50 years
of age, living in 7 of the 8 reported
counties along the Texas-Mexico
border, were higher than the state
and national rates for Hispanic
men of similar age. Additionally,
there was an upward trend in the
incidence of CRC in Hispanics
males ≥50 years of age living in El
Paso County. In contrast, the rate of
CRC declined or remained stable in
Non-Hispanic Whites and women at
the state and national level. (Tables
1 and 2).
DISCUSSION
Our study unveils a significant
disparity in the incidence of CRC by
ethnicity and place of residence. Of
note, most cancer databases and
published literature report data for
Hispanics as an aggregate group,
which can be masking differences
among Hispanic subpopulations.
While the majority of US Hispanics
are of Mexican origin, the population
is not evenly distributed across the
US;4 there is a heavier concentration
residing near the US-Mexico
border. Our study may suggest that
Hispanics of Mexican origin may
be disproportionately affected by
CRC, or Hispanics living in border
communities have different risk
profiles.
(Additional details for El Paso County presented in Table 1).
continued on page 20 ►►