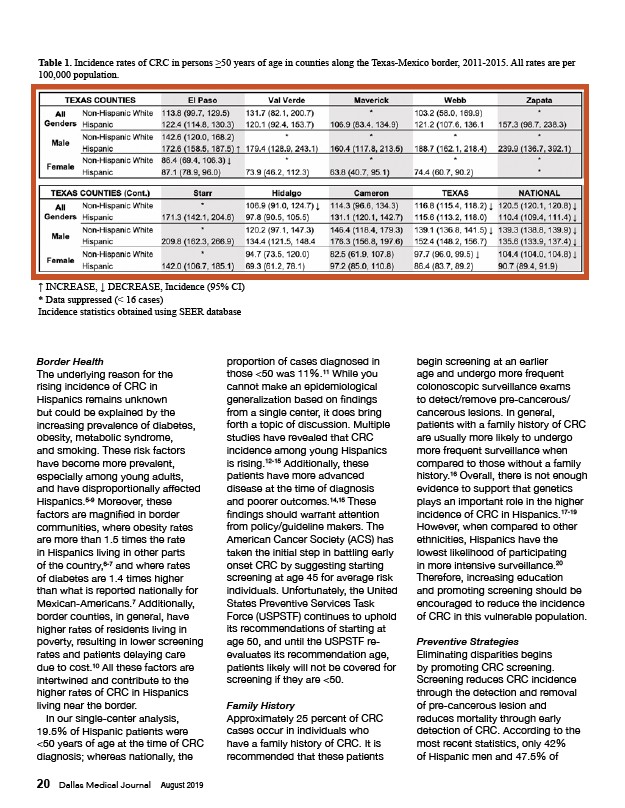
Table 1. Incidence rates of CRC in persons ≥50 years of age in counties along the Texas-Mexico border, 2011-2015. All rates are per
100,000 population.
↑ INCREASE, ↓ DECREASE, Incidence (95% CI)
* Data suppressed (< 16 cases)
Incidence statistics obtained using SEER database
Border Health
The underlying reason for the
rising incidence of CRC in
Hispanics remains unknown
but could be explained by the
increasing prevalence of diabetes,
obesity, metabolic syndrome,
and smoking. These risk factors
have become more prevalent,
especially among young adults,
and have disproportionally affected
Hispanics.5-9 Moreover, these
factors are magnified in border
communities, where obesity rates
are more than 1.5 times the rate
in Hispanics living in other parts
of the country,6-7 and where rates
of diabetes are 1.4 times higher
than what is reported nationally for
Mexican-Americans.7 Additionally,
border counties, in general, have
higher rates of residents living in
poverty, resulting in lower screening
rates and patients delaying care
due to cost.10 All these factors are
intertwined and contribute to the
higher rates of CRC in Hispanics
living near the border.
In our single-center analysis,
19.5% of Hispanic patients were
<50 years of age at the time of CRC
diagnosis; whereas nationally, the
20 Dallas Medical Journal August 2019
proportion of cases diagnosed in
those <50 was 11%.11 While you
cannot make an epidemiological
generalization based on findings
from a single center, it does bring
forth a topic of discussion. Multiple
studies have revealed that CRC
incidence among young Hispanics
is rising.12-15 Additionally, these
patients have more advanced
disease at the time of diagnosis
and poorer outcomes.14,15 These
findings should warrant attention
from policy/guideline makers. The
American Cancer Society (ACS) has
taken the initial step in battling early
onset CRC by suggesting starting
screening at age 45 for average risk
individuals. Unfortunately, the United
States Preventive Services Task
Force (USPSTF) continues to uphold
its recommendations of starting at
age 50, and until the USPSTF reevaluates
its recommendation age,
patients likely will not be covered for
screening if they are <50.
Family History
Approximately 25 percent of CRC
cases occur in individuals who
have a family history of CRC. It is
recommended that these patients
begin screening at an earlier
age and undergo more frequent
colonoscopic surveillance exams
to detect/remove pre-cancerous/
cancerous lesions. In general,
patients with a family history of CRC
are usually more likely to undergo
more frequent surveillance when
compared to those without a family
history.16 Overall, there is not enough
evidence to support that genetics
plays an important role in the higher
incidence of CRC in Hispanics.17-19
However, when compared to other
ethnicities, Hispanics have the
lowest likelihood of participating
in more intensive surveillance.20
Therefore, increasing education
and promoting screening should be
encouraged to reduce the incidence
of CRC in this vulnerable population.
Preventive Strategies
Eliminating disparities begins
by promoting CRC screening.
Screening reduces CRC incidence
through the detection and removal
of pre-cancerous lesion and
reduces mortality through early
detection of CRC. According to the
most recent statistics, only 42%
of Hispanic men and 47.5% of