form a dedicated team of core specialists to
optimize infection control measures in the
shelter.
Th is innovative infection prevention
team consisted of infection control
experts (infectious disease physicians and
hospital infection prevention nurses)
who served daily eight-hour shifts at the
shelter beginning Sept. 3. Th ey applied
their practical experience in hospital
settings to this shelter setting by providing
education and training materials to clinic
and general shelter staff and residents;
creating cleaning, disinfection, testing,
722
498
228
215
204
130
73
72
64
64
58
53
46
44
25
23
19
12
8
96
and isolation protocols for the clinic;
developing infection prevention rounding
tools to ascertain whether critical general
shelter areas (e.g., daycare, food-service,
bathrooms, showers, linens areas) were
checked regularly and gaps addressed;
meeting with cleaning agencies to ensure
that eff ective products and procedures were
used; monitoring hand hygiene and related
supplies in the shelter and clinic; and
administering infl uenza vaccinations.
Ultimately a few cases of scabies and
lice were diagnosed in the clinic, as well
as one patient who had PCR-confi rmed
12 Dallas Medical Journal December 2017
norovirus and one with PCR-confi rmed
infl uenza A. Th e success of the rigorous
infection prevention and control eff orts was
demonstrated by the absence of outbreak
numbers of these illnesses, in our largescale
shelter setting where transmission
could easily have been perpetuated.
Th rough the four weeks of the Hurricane
Harvey sheltering response in Dallas, we
were fortunate to be able to draw from
our local sheltering experiences from prior
hurricanes, and to have the support of city,
county, state, and federal agencies to ensure
the resources necessary for implementation
of current standards of practice. We also
are thankful for the generous volunteer
spirit of our healthcare community. Th eir
enthusiastic donation of time and expertise
made it possible to not only care for the
needs of those directly impacted by this
crisis, but to additionally seek innovative
approaches and impro vements for future
disaster responses. DMJ
Acknowledgements
We thank the following people for their
work on the Data Management team:
Kyoo Shim, MPH; James Blackwell, MPH;
Michelle Ward, MPH; Joel Henderson,
MPH; Sonya Hughes, MPH; Meredith
Stocks, MPH; Folasuyi Richardson, MPH;
Peter Binoj, MPH; Angela Mihalic, MD,
Andrew Tran and UT Southwestern
Medical School students; Cristie Columbus,
MD, and Texas A&M College of Medicine
students; Bijal Balasubramanian, PhD, and
UT Houston School of Public Health Dallas
Campus students.
We thank the following people for
their work on the Infection Prevention
team: Trish Perl, MD; Julie Trivedi, MD;
Carolee Estelle, MD; Pranavi Sreeramoju,
MD; Michael Sebert, MD; Pat Metcalf
Jackson, RN, Children’s Health Dallas
Infection Prevention; Doramarie Arocha,
PhD, Elizabeth Th omas, Cari Stebbins,
Chris Henderson, Bethany Philips, UTSW
Clements Hospital Infection Prevention;
Karla Voy-Hatter, RN, Jennifer Ochieng,
Latitia Houston, Dena Taherzadeh,
Parkland Hospital Infection Prevention;
Cheryl Sharp, Deepika Manandhar, Nicki
Andrews, Prinu Gabriel, Texas Health
Resources Infection Prevention; Neeraja
Ganeshraj, Baylor Scott & White Health
Infection Prevention; Benjamin Walker,
Methodist Charlton Infection Prevention;
Glenda Nelson; Cathy Grayson; and Sheila
Culver.
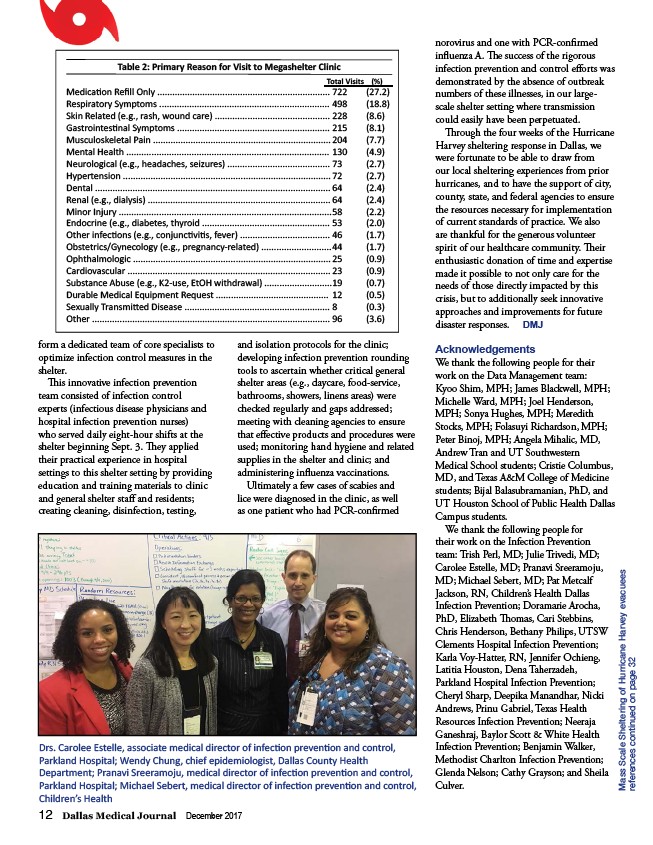
Drs. Carolee Estelle, associate medical director of infecti on preventi on and control,
Parkland Hospital; Wendy Chung, chief epidemiologist, Dallas County Health
Department; Pranavi Sreeramoju, medical director of infecti on preventi on and control,
Parkland Hospital; Michael Sebert, medical director of infecti on preventi on and control,
Children’s Health
Mass Scale Sheltering of Hurricane Harvey evacuees
references continued on page 32
Medicati on Refi ll Only .....................................................................
Respiratory Symptoms ....................................................................
Skin Related (e.g., rash, wound care) ..............................................
Gastrointesti nal Symptoms .............................................................
Musculoskeletal Pain .......................................................................
Mental Health .................................................................................
Neurological (e.g., headaches, seizures) .........................................
Hypertension ...................................................................................
Dental ..............................................................................................
Renal (e.g., dialysis) .........................................................................
Minor Injury .....................................................................................
Endocrine (e.g., diabetes, thyroid ...................................................
Other infecti ons (e.g., conjuncti viti s, fever) ....................................
Obstetrics/Gynecology (e.g., pregnancy-related) ............................
Ophthalmologic ...............................................................................
Cardiovascular .................................................................................
Substance Abuse (e.g., K2-use, EtOH withdrawal) ...........................
Durable Medical Equipment Request .............................................
Sexually Transmitt ed Disease ..........................................................
Other ...............................................................................................
(27.2)
(18.8)
(8.6)
(8.1)
(7.7)
(4.9)
(2.7)
(2.7)
(2.4)
(2.4)
(2.2)
(2.0)
(1.7)
(1.7)
(0.9)
(0.9)
(0.7)
(0.5)
(0.3)
(3.6)
Table 2: Primary Reason for Visit to Megashelter Clinic
Total Visits (%)